Transplant physicians face the challenge to detect allograft rejection using non-sensitive biomarkers and clinical signs/symptoms.
For kidney transplant, serum creatinine, urinalysis for proteinuria or hematuria, are so far used for screening for rejection and/or assessment of graft function. In a recent article in Sci Transl Med, De Vlaminck et al. investigated the use of cell-free circulating DNA (cfdDNA) as a marker of allograft rejection in adult heart transplants.
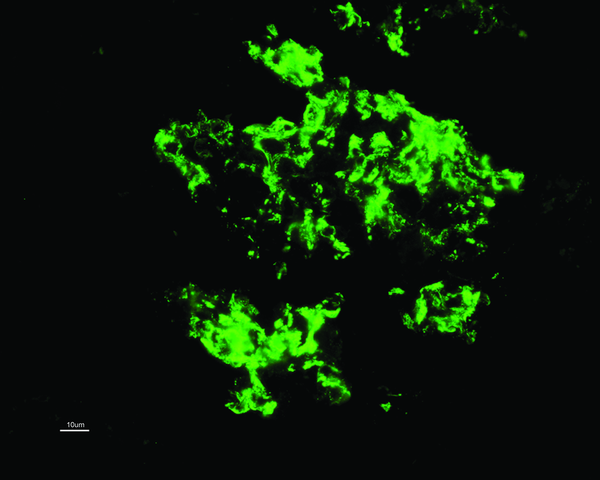
Authors used shotgun sequence approach to detect donor-specific DNA fragments (SNP genotyping), and correlated the level of cfdDNA with cardiac biopsy results, the diagnostic “gold standard” for rejection.
The idea of a “liquid biopsy” —using plasma circulating DNA fragments—as a diagnostic tool has been explored in the Oncology field, to detect early and late stage cancers.
In transplant field, the presence of donor-derived DNA fragments in recipient’s plasma (or urine), called microchimerism, has been known since the end of 1990s and using them as a measure of transplant injury has been tried. For example, Sidgel et al. used Y-specific DNA fragments as a marker in male-to-female transplants.
In this current article, De Vlaminck et al. further improved this approach to overcome dependency on donor-recipient pair. Authors concluded that using the cutoff value of 0.25%, cfdDNA method is as sensitive (0.58) and specific (0.87) as biopsy (0.58 and 0.96, respectively). Furthermore, cfdDNA approach was able to detect rejection as early as 5 months prior to tissue diagnosis.
There are, of course, some limitations to overcome: 1) cfdDNA cannot differentiate ACR vs AMR, 2) cannot rule out other source of DNA fragments, such as endothelial damage without rejection 3) exhibit still substantial discordance with biopsy results. Although currently using the shotgun approach, the technique can be refined by using targeted-sequencing approach, to be less laborious process.
Based on the same underlying principles, it is very likely that similar test would have application in kidney transplantation and potentially help to detect earlier ongoing graft injury. We will still need the biopsy though to clarify the type of injury...
Naoka Murakami